



The hand is anatomically complex. Having an anatomical-based approach to the assessment of patients who present to the Emergency Department is important to preserve quality of life following a hand injury. Hand injuries are the second most common injury leading to days without work. It is no surprise then that open finger injuries land in the top 10 most common diagnoses that end up in court. In this first part of our two-part series on hand injuries Dr. Matt Distefano and Dr. Arun Sayal guide us through the principles and pitfalls of assessment and management of hand injuries and answer questions such as: what is the differential diagnosis of a globally swollen hand? What is the intrinsic minus hand position? When should we suspect compartment syndrome of the hand? How should we best locate retracted lacerated tendons of the hand? What are the best ways to control bleeding of a finger tip amputation? What are the best analgesic choices? How large of a skin avulsion hand injury should we let heal by secondary intention rather than recommend a flap/skin graft? and many more…
Podcast: Play in new window | Download (Duration: 1:06:08 — 60.6MB)
Podcast production, sound design & editing by Anton Helman, voice editing by Braedon Paul
Written Summary and blog post by Kate Dillon & Ian Beamish, edited by Anton Helman January, 2023
Cite this podcast as: Helman, A. Sayal, A. Distefano, M. Episode 178 Hand Injuries – Pitfalls in Assessment and Management. Emergency Medicine Cases. January, 2023. https://emergencymedicinecases.com/hand-injuries-assessment-management. Accessed September 6, 2024
3 key points to keep in mind when approaching hand injuries:
Essential hand anatomy overview video: https://www.youtube.com/watch?v=zyl6eoU-3Rg
Mnemonic for carpal bones: So Long To Pinky, Here Comes The Thumb
Hand dominance and vocation/recreation
Mechanism of injury
Clinical Pearl: The mechanism of injury should not only guide your physical exam, but immediately generate a list of possible complications. Retained foreign body, joint space violation, tendon injury, bacterial infection, tetanus, rabies, high pressure injection injury complications, and compartment syndrome need to be front of mind.
Comorbidities
For access to all talks and video streaming package from EM Cases Summit visit https://emcasessummit.com/
As with all orthopedic injuries, be methodical in your exam and ensure you look, feel, move, and then do some special tests when indicated.
1.Look
Inspect for swelling, erythema, atrophy, deformity, skin changes, abnormalities in the lie of the hand and always inspect the contralateral limb to understand what’s normal for the patient. Some things to look out for include:
Signs of vascular injury – active bleed, expanding mass, poor capillary refill time, pallor, global hand swelling
Cascade of the fingers – with the hand resting with palmar surface up, from the 2nd digit to 5th there should be a subtle increase in flexion and any abnormality in this transition usually represents an underlying pathology; for example, looking at the palmar surface and noticing one finger fully extended suggests a flexor tendon injury

Normal resting hand cascade
Pitfall: one of the often-missed deformities in the hand is a rotational deformity, remember to look at the cascade of the hand in neutral and compare it to the other side so that you do not miss subtle scissoring of the digits
2.Feel and Move
Palpate for a pulse! Vascular supply to the hand has lots of redundancy and can be well supplied by the radial artery alone, or the ulnar artery alone so we usually have some room here. Our experts do not see a need to assess collateral circulation with the Allen Test.
Clinical Pearl: The radial artery runs more superficially than the ulnar artery, so it is the radial artery that we most often see damaged in a laceration injury.
Pitfall: Be very careful when handling the cut end of arteries to ensure we give our surgical colleagues the best chance to repair them. When tying them off to stop a bleed, leave your sutures long!
Next, feel where they have pain and then order the correct X-ray (finger pain = finger X-ray, not hand!) and use your clinical exam to guide your eyes when reviewing imaging.
3.Neuro Testing in the Hand
Median nerve – sensation tip of 2 nd digit palmar side, motor testing with making a fist
Radial nerve – sensation to 1 st dorsal web space, motor testing with thumbs up
Ulnar nerve – sensation tip of 5 th digit palmar side, motor testing with peace sign
Digital nerves – two-point discrimination is gold standard, but can just use pinpick/light touch to screen.
Special Test: Froment’s sign
Froment’s sign is the inability to keep thumb and index finger straight when trying to pinch a piece of paper. This represents weakness of loss of function of adductor pollicis representing ulnar nerve damage (flexor pollicis brevis takes over, which is supplied by the median nerve).

Froment’s sign – notice the left thumb DIP flexes to compensate for defective adductor function
Flexors
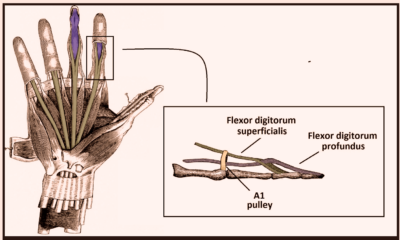
Flexor Digitorum Superficialis (FDS)
Originates from 4 unique muscles and splits over the PIP joint and inserts at base of middle phalanx. To test FDS function eliminate the FDP by holding 3 of the patient’s digits in complete extension, the digit in question will no longer be able to flex at the DIP and we can now test FDS which will be acting in isolation to flex at the PIP.
Flexor Digitorum Profundus (FDP)
Originates from one muscle belly and runs underneath FDS to insert at the base of distal phalanx (runs over both PIP + DIP). To test function of FDP, simply hold down middle phalanx and ask the patient to flex at the DIP

Testing the FDS and FDP
Clinical Pearl: 15% of people have an independent FDP to their index finger. 8-10% do not have an FDS to their 5 th finger. Always check the other hand to see what is normal for the patient.
Pitfall: Ensure a graded approach to resistance testing because being too aggressive right off the bat can lead to rupture of that last 5% of a partially torn tendon which makes healing and repair more difficult.
Extensors
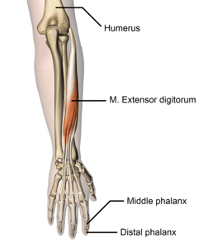
Assessing for central slip rupture with the Elson test
The central slip originates from the long extensors from the forearm to the fingers and inserts across the PIP. However, lateral branches originating from the same long tendon branch out to flank the PIP and insert distally across the DIP. Therefore, ask the patient to extend the PIP joint against resistance from a 90 degree flexed position over the edge of a table; then assess the resistance of the DIP joint to flexion. This is called the Elson test. It is positive if there is weak extension force at the PIP with fixed extension at the DIP.
If you cannot see a tendon at the laceration site, ensure good lighting (our experts keep a cheap camping headlamp nearby at all times), have an assistant available to help retract and then look for the cut end of the tendon with mosquito forceps. The tendon usually retracts proximally. If you can, pull it distally within the sheath and tack it down with a quick suture – this will help later for definitive repair.
There are ten muscular compartments of the hand plus the carpal tunnel. Diffuse swelling of the hand is compartment syndrome (in multiple compartments) until proven otherwise. The carpal tunnel warrants special mention, although it is neither a muscular nor a fascial compartment of the hand. This closed space has the potential to develop acute carpal tunnel syndrome (a kind of compartment syndrome) if it is filled with blood, which occurs in approximately 10-15% of distal radius fractures.

Intrinsic Minus hand position with extension at the MCPs and IP joint flexion
Intrinsic Plus Position is a position of the hand that assumes that the intrinsic muscles of the hand (muscles that start and end in the hand) are functioning properly. The intrinsic muscles (lumbrical muscles) are responsible for isolated flexion of the MCP joints.
Intrinsic Minus Position (“claw hand”): conversely this assumes that the lumbricals are not functioning properly. In this position the MCPs are neutral or slightly extended and the IP joints are in flexion. This is the most consistent physical exam finding in compartment syndrome of the hand.
Besides direct pressure and elevation, finger tourniquets may be helpful to achieve hemostasis. Three options include using the finger of a clean latex glove, proprietary finger tourniquets and a Penrose drain wound around the base of the finger (see images below). After the tourniquet is applied have the patient milk out the blood from the finger. As the hand is incredibly well vascularized a finger tourniquet can be safely left in place for up to 45 minutes.
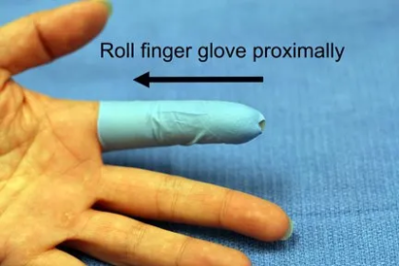

Glove tourniquet technique for hemostasis

Penrose drain finger tourniquet
Pitfall: do not suture, ligate or clamp bleeding arteries in the finger, as the nerves run very closely to the arteries portending a risk of pinching/ligating a nerve inadvertently.
The main principle for analgesia in the hand is do what you are comfortable and good at doing. There are many ways to anesthetize the hand including regional blocks, field blocks, single or combination nerve blocks and Bier blocks. Our experts utilize the subcutaneous nerve block (single palmar injection) for digital blocks (see image and description below). Two small prospective studies demonstrated that there were similar efficacies of patient analgesia and patient satisfaction between single volar blocks and traditional 2-injection dorsal digital blocks. Remember to use small gauge needles to reduce discomfort.
Subcutaneous single volar injection digital block

Pitfall: a common pitfall is unnecessary prolonged immobilization of the hand which may result in chronic stiffness, contractures and dysfunction
Position of safe immobilization
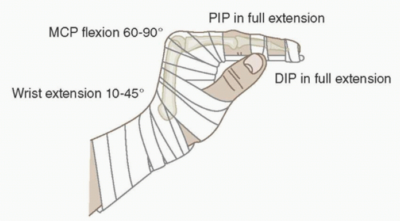
The position of safe immobilization allows the soft tissues to be at maximum length with the wrist in slight extension, the MCPs in 90 degrees flexion and the IP joints straight in extension.
Pearl: if a skin avulsion defect is less than the size of a dime, let it heal by secondary intention rather than attempting a flap/skin graft
Pitfall: a common pitfall is not splinting proximally enough; the tendons that function in the hand originate at the elbow or in the forearm, so a laceration of an extensor tendon should be splinted from the fingertips to the elbow
Drs. Helman, Sayal and Destefano have no conflicts of interest to declare
Now test your knowledge with a quiz.